Fogarty funding spurs global health innovations
November / December 2013 | Volume 12, Issue 6
In an attempt to create "mini-Manhattan Projects," Fogarty is funding multidisciplinary teams to identify thorny global health problems and take solutions-based approaches to resolve them. Several grantees shared their ongoing efforts at a recent NIH meeting. Examples included novel architectural and engineering measures to combat tuberculosis and an inexpensive diagnostic tool to reduce malaria in low-resource settings.

Photo by Susan Urmy/Vanderbilt University
The pictured tool, developed with support from
Fogarty's Framework Programs for Global Health
Innovation, uses tiny magnets and plastic tubing to
prime blood samples for malaria testing in
low-resource areas.
Watch a demonstration of the Extractionator tool
[video] developed by the Fogarty-supported
Vanderbilt University team.
Fogarty's Framework Programs for Global Health Innovation encourages multidisciplinary research and training aimed at developing new products, processes and policies to solve health problems in low- and middle-income countries (LMICs). The initiative supports joint training for U.S. and developing country researchers as they brainstorm possible solutions, conduct research to validate their concepts, implement successful approaches and bring them to scale. So far, Fogarty has awarded 10 Framework Innovation grants, totaling nearly $16 million over five years.
"Not all of the innovation projects will succeed but it is our intention that, by going through this process, the participants will learn to think more creatively and gain experience bringing different disciplines to bear on a single problem," said Fogarty's Dr. Flora Katz, who's overseeing the program. "Our definition of innovation in this context is the translation of a new idea into significant and positive change."
Developing low-cost malaria diagnostics
Malaria is notoriously difficult to diagnose, especially in low-resource settings without ready access to lab equipment. A key problem is hidden infection in asymptomatic people. They don't seek treatment so mosquitoes biting them can transfer Plasmodium falciparum parasites to people nearby. Identifying and treating these malaria reservoirs requires a sensitive diagnostic test, but existing products are either too expensive, unable to detect low infection levels or require highly trained lab assistants.
A Framework grant awarded to Drs. David W. Wright, Frederik Haselton and Douglas Heimburger at Vanderbilt University is enabling a dozen American and Zambian research trainees to develop and deploy novel solutions for this critical issue. A new inexpensive test would improve the likelihood of detecting infection and also reduce drug resistance in the parasite by treating only those who harbor it instead of blanket-treating anyone with a fever, which commonly occurs in malaria endemic countries.
Wright's lab previously developed a related low-cost tool that primes blood samples for malaria testing. In their prototype, a minimally trained operator places a few drops of blood into the end of a small plastic tube over a cluster of tiny magnetic beads that attract molecules from the malaria parasite. The operator then uses a handheld magnet to draw the beads down the tube through several prefilled chambers that cleanse the sample for testing. This project was supported by the Bill and Melinda Gates Foundation.
Zambia is trying to eliminate the parasite within its borders but its campaign has met with patchy success. The Framework researchers will combine their skills in basic science, engineering and public health science and rethink how to detect the parasites in humans. If their investigations produce potentially marketable ideas, the cohorts will conduct field tests in Zambia for six months, evaluating how well the new technologies perform in areas of high, medium and low parasite density.
Zambia would retain intellectual property rights and licenses for any products developed by the Framework trainees, potentially generating a long-term revenue source. Multiple Zambian partner institutions are supporting the research, including the Malaria Institute at Macha, the University of Zambia, the National Malaria Control Centre and the Tropical Diseases Research Centre.
Partnering with architects to combat TB
The spread of drug-resistant TB is a growing concern and poses a serious problem in confined, crowded spaces such as hospitals, clinics, prisons and refugee camps. A Framework grant led by Dr. Edward Nardell at Brigham and Women's Hospital in Boston is bringing together architects and engineers with infectious disease researchers and others to study new ways to slow the spread of TB.

Photo by Alan Ricks/MASS Design Group
Fogarty Framework Innovation grantees are bringing
architects and engineers together with infectious
disease researchers and others to study new ways to
slow the spread of TB in developing countries.
The work is drawing inspiration from a previous project in Rwanda, where the nonprofit MASS Design Group designed a new hospital specifically to minimize airborne TB spread. They located it on the top of a hill to maximize natural airflow, incorporated plenty of windows for cross-ventilation, changed the ward layout, added large fans and installed ultraviolet lights to deactivate TB bacteria. The project was a collaboration with the nonprofit Partners in Health and the country's health ministry.
With the Framework grant, Nardell and his colleagues will guide trainees in South Africa and Peru as they look for fresh approaches to combat TB. The work is supported in part by the NIH Office of Disease Prevention.
In South Africa, teams will study ways to curb Mycobacteria tuberculosis transmission, including developing and testing novel indicators of successful building designs and novel disinfection technology. If the innovations show promise, the teams will work with collaborators to refine and market the products in a sustainable way. Contributing to the project are Partners in Health, the University of Pretoria Architecture Department and several other South African organizations.
In Peru, Framework trainees plan to test a novel way to diminish the risk that infectious patients pose to others while waiting to be seen by medical staff. Researchers will survey visitors to hear who has coughs that might indicate TB and will collect their samples for rapid molecular tests to confirm infection and to identify drug resistant pathogens. Infected patients will immediately receive appropriate treatment. Partners in this project are Peru's Hospital Nacional Hipolito Unanue and Socios En Salud.
Using novel ceiling design to reduce TB transmission
Eggcrate ceiling panels combined with off-the-shelf ultraviolet radiation lamps and ceiling fans can dramatically reduce bacteria in indoor air, Nardell and a team of Framework researchers has discovered.
In their study, they cut bacterial density by up to 90 percent with a low-cost ceiling design that improved airflow, enabled greater UV lamp efficiency and demonstrated a new way to shield people from UV radiation.
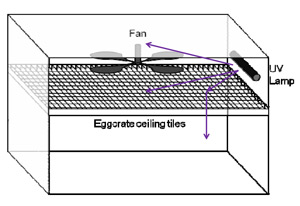
Illustration courtesy of Dr. Jacqueline Linnes/Harvard
Fogarty-supported researchers used a low-cost
ceiling design, illustrated above, to improve airflow
and reduce TB transmission.
The results were published recently in the Indoor Air journal. (Read about the article Eggcrate UV: a whole ceiling upper-room ultraviolet germicidal irradiation system for air disinfection in occupied rooms.) Nardell, Dr. Stephen Rudnick and their colleagues found they could kill TB and other bacteria which collect in the upper part of rooms, without resorting to expensive ventilation or air filtration systems that can be noisy, ineffective and often short-circuit. UV radiation lamps successfully kill germs, but to protect people from related eye and skin irritation the lamps are typically hidden behind louvers that reduce airflow and limit the germicidal impact.
The researchers substituted solid ceiling panels with crosshatched, eggcrate panels, suspending them to improve airflow and doubling up panel layers near the lamps or angling their placement to keep people shielded. They also installed a ceiling fan to improve air circulation between the upper and lower sections of the room. Air quality tests showed this design cut bacterial density by 82-90 percent, whereas conventional methods only reduced them by 37-67 percent.
Although UV germicide irradiation has been used for over 60 years, this is the first major advance in its application, according to the authors.
In addition to Fogarty, the National Institute for Occupational Safety and Health and Harvard Education and Resource Center supported the project.
More Information
To view Adobe PDF files,
download current, free accessible plug-ins from Adobe's website.