African experts share COVID-19 contact tracing tips
September / October 2020 | Volume 19, Number 5
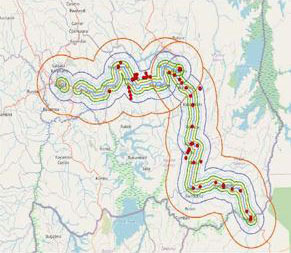
Image courtesy of Dr. Sabin Nsanzimana
Rwanda’s COVID-19 response included using a GPS app
to monitor and conduct contact tracing of truck drivers.
By Susan Scutti
African nations have recorded lower rates of COVID-19 than many high-income countries, which is attributable, some say, to the continent’s robust public health response. Several leaders of coronavirus response teams in Africa presented
best practices of contact tracing in a recent webinar co-moderated by Dr. Jean Nachega of the African Forum for Research and Education for Health's (AFREhealth) and Fogarty’s Deputy Director Dr. Peter Kilmarx, and organized by Fogarty’s Dr. Cecile Viboud. Presenters from Nigeria, South Africa, Uganda and Rwanda said their countries responded to the pandemic with largely similar measures, and transitioned from centralized contact tracing efforts to decentralized models over time.
Nigeria leveraged community networks established in response to Lassa fever and Ebola, said Dr. Rhoda Atteh, leader of her nation’s COVID operation center. Contact tracers primarily relied on in-person interviews - not phone calls - to connect the dots between Nigeria’s confirmed and suspected cases. “We focus on doing self-isolation at home and also monitoring contacts remotely,” she said, acknowledging that it’s been difficult to assess adherence. “There's a lot of misinformation and stigma around COVID-19,” said Atteh, who heard reports of contact tracing teams being attacked. “For a lot of cases identified, not a single contact is actually traced,” said Atteh. More community engagement, both before and during the contact tracing process, would improve Nigeria’s response, she suggested.
When the virus began to circulate in Uganda, the government activated an incident management system, according to Dr. Alex R. Ario, of the country’s National Institute of Public Health. Non-pharmacological interventions combined with regional contact tracing helped interrupt the country’s outbreak. Regional teams linked with the incident management operation to maintain communication with laboratories and case management workers, explained Ario, noting that “established community systems” required less expense and were more efficient than a centralized approach. Uganda’s Village Health Teams not only contact trace, they also follow-up with patients discharged from isolation and quarantine; distribute health commodities, including sanitizers and medicines; conduct COVID-19 community disease surveillance; provide health education; and collect data for other health conditions, he explained.
In Rwanda, pandemic-related public health measures included handwashing stations, face-masking and physical distancing. A national preparedness and response command post managed epidemiology surveillance, case management, laboratory operations, data science, logistics, communications and administration, said Dr. Sabin Nsanzimana, director of Rwanda’s Biomedical Centre. An advisory group of Rwandan scientists also provided data and evidence-based recommendations. Nearly 20,000 contacts have been traced and checked, he said, noting some contacts were not accessible but “they're not many.” To decentralize contact tracing efforts, Rwanda adapted “a complexity of IT solutions,” he added. This includes a geospatial mapping system, an IT notification system previously used in the HIV program, an electronic tool for conducting home-based monitoring and a GPS app for truck drivers. Stigma was a problem initially, yet as people came to better understand the disease, “this is no longer an issue,” said Nsanzimana.
In South Africa, the government declared a national disaster followed by travel restrictions, distancing measures and a coronavirus testing program. Drs. Hassan Mahomed and Masudah Paleker coordinated contact tracing in Western Cape Province. Paleker, who believes geography itself posed a challenge to contact tracing in a province with rural and urban areas, said “we started a decentralized process from quite early on.”
Preexisting district teams drove the effort aided by the provincial health department. A single patient viewer (SPV) electronic database was repurposed to conduct contact tracing and case reporting due to its accessibility and sorting capabilities. The health department developed two additional applications for monitoring symptoms and uploading contact details.
“Both of these applications had fairly limited uptake by the population, although they were quite actively promoted,” said Mahomed. Isolation facilities were also underused, “partly because of stigma, partly because of fear of loss of a position or what would happen to their homes,” he said, while anecdotal reports suggest low adherence to quarantine measures. Still, Mahomed said he believes the SPV database was crucial to the outbreak response, while best practices include community preparation and planning, and population-based infection control practices. He added that South Africa is preparing for future waves of the disease. “Our current strategies are to be agile and scalable in order to respond quickly.”
Dr. Jay Varma had been working in Africa since 2017 to help create the new African CDC when he was called back to New York City in March to provide guidance on the city’s coronavirus response. He summarized contact tracing best practices, noting the same principles would apply to infectious disease preparedness on both continents. “First and foremost, the single most important determinant of success [during a public health emergency] is political commitment,” he said, adding that responsibility must extend from highest to lowest government levels. “The next most important is funding.”
Rapidly scaling up contact tracing posed a “tremendous challenge” in both the U.S. and Europe, where infectious disease crises are less frequent, said Varma. “Public health emergencies are almost like muscles for physical health – if you don't use them repeatedly, you will lose them.” Choosing appropriate technologies also complicated New York’s COVID-19 response, he said. Data may be scalable, easy to use and able to function in low bandwidth settings, but “everybody” in the U.S. wants to “make sure you have a system that can apply to every situation,” said Varma. “Choosing a rapid solution that is likely to be effective quickly often loses, because people raise questions such as: How is it going to solve these five other problems?”
Varma also noted that “there is tremendous variability across the entire world in the rapidity and ease with which people have access to diagnostic testing.” New York City “dramatically” increased testing to about 45,000 PCR tests per day - approximately 5 for 1,000 people, which is around the level of South Korea at its peak - yet most areas of the world could never offer similar high capacity testing, he said. “We have to think about the effectiveness of contact tracing in settings where testing is not widely available.”
“The successes of Africa really need to be told,” said Varma, adding that “strong commitment, strong social cohesion and an ability to recognize how to adapt solutions at a broad scale - these are critical lessons that Africa needs to be able to teach the rest of the world.”
“It's humbling and impressive to see the kind of response that has been stood-up across countries in Africa,” concluded Dr. Mike Reid, University of California, San Francisco. “We have huge amounts to learn from what you're doing.”
More Information
-
Contact tracing and the COVID-19 response in Africa: Best practices, key challenges, and lessons learned from Nigeria, Rwanda, South Africa, and Uganda [Open access], co-authored by Fogarty's Drs Cecile Viboud and Peter H Kilmarx
The American Journal of Tropical Medicine and Hygiene, February 11, 2021 - Recorded webinar:
Contact tracing in the COVID-19 response: Best practices in Africa [Video]
Presented by AFREhealth and Fogarty, October 5, 2020 -
Prioritizing research training and medical education in Africa
Q and A with Dr Jean Nachega
Jan / Feb 2020
Global Health Matters -
Dr Peter Kilmarx appointed Fogarty Deputy Director
Fogarty news, July 30, 2015 -
Profile: Dr. Hassan Mahomed
University of Cape Town via academica.edu -
Public health medicine registrars
Division of Health Systems and Public Health, Stellenbosch University -
Dr. Ario leading ministry's team of epidemiologists against COVID-19
New Vision, August 5, 2020 -
Biography: Dr. Sabin Nsanzimana
Rwanda Biomedical Center -
Biography: Dr Jay Varma
Africa CDC
To view Adobe PDF files,
download current, free accessible plug-ins from Adobe's website.
Related World Regions / Countries