In an increasingly interconnected world, the health of Americans is impacted by scientific advances that take place in every region of the globe. Through partnerships between U.S. investigators and their collaborators in other countries, we can leverage the best talent to address common health challenges that affect Americans as well as populations abroad. New technologies and innovations developed in other countries offer particularly exciting opportunities to improve the health of Americans across all ages and conditions. To help realize these possibilities, Fogarty invests in strengthening global health scientific expertise in the U.S. and abroad and facilitates mutually beneficial research partnerships between international and U.S. investigators. At NIH, this role and mission are unique to Fogarty.
Benefits from these investments include advancing our understanding of both communicable and non-communicable universal health threats, such as Alzheimer's disease, heart disease, and cancer; detecting, containing, and minimizing outbreaks at their point of origin; studying diseases in populations where they are prevalent; and applying rigorous scientific methods to learn from prevention strategies or treatments used in other countries.
Fogarty supports U.S. investigators across the nation. In FY24, Fogarty funded 440 US grantees from 122 US institutions in 39 states, including the District of Columbia. These grants increase the reach and competitiveness of the U.S. and its universities by offering training opportunities for American scientists abroad and fostering global collaborations. These collaborations result in long-term relationships that provide scientific and training opportunities for U.S. and international partners, help American scientists remain at the forefront of scientific discovery, and strengthen the research capacity of their international partners. In addition, early-career U.S. and international scientists who started their academic career through Fogarty-funded training often go on to receive research support from other NIH Institutes and Centers and train the next generation of global health scientists and innovators.
Ultimately, the researchers and research networks supported through Fogarty grants can propel scientific progress forward in ways that can benefit the American people now and in the future. Many FIC-trained scientists have made and continue to make critical contributions to global public health challenges that affect us all.
Investing in leaders who make discoveries with impact in the US and abroad
 Volunteers in Guinea, wearing full personal protective equipment, disinfect themselves after working in the field with material exposed to Ebola virus.
Volunteers in Guinea, wearing full personal protective equipment, disinfect themselves after working in the field with material exposed to Ebola virus.
1. Using genomic sequencing for early detection of Ebola virus
Fogarty-trained researchers use innovative technology and skills in genomic sequencing gained during their training to track diseases such as cholera, malaria, dengue, and Ebola more quickly, before they become global threats. Dr. Christian Happi is a past recipient of the Fogarty International Research Collaboration Award and the former principal investigator on the NIH’s Human Heredity and Health in Africa (h6Africa) project. Dr. Happi helped establish the African Center of Excellence for Genomics of Infectious Diseases (ACEGID) at Redeemer’s University in Nigeria, the first infectious disease genomics platform in West Africa. He has used genomics technology for early diagnosis and confirmation of Ebola virus disease in Nigeria, which saved millions of lives during the Western Africa epidemic of 2013-2016 and helped prevent the disease from becoming a major public health threat in the US.
2. Fogarty-supported/trained scientists in Boston and Pittsburgh identify new SARS-CoV-2 and mpox variants
When COVID-19 pandemic broke out in Botswana, Dr. Sikhulile Moyo, former trainee of Fogarty’s Fellows and Scholar program, was quick to pivot his work that utilized genomic sequencing to study HIV/AIDS and other diseases to the new health threat. He and his team at Botswana Harvard AIDS Institute observed a previously unseen pattern of mutations among the SARS-CoV-2 samples collected in mid-November 2021. Researchers deposited the sequences into the international pathogen database. The WHO’s virus working group classified them as a new SARS-CoV-2 “variant of concern.” Rapid identification of a new infectious variant close to its source bought responders in Botswana and abroad precious time to develop countermeasures. Similarly, funding from the Medical Education Partnership Initiative, cofounded by Fogarty, allowed Dr. Jean Nachega of University of Pittsburgh and his colleagues to identify the epidemiological and genomic features of an mpox outbreak in eastern Democratic Republic of the Congo that was caused by the new clade of the virus.
Harnessing technology and innovation to improve health care delivery
1. Developing low-cost diagnostics for early cancer detection
Fogarty grant recipient Dr. Dongkyun Kang of Massachusetts General Hospital developed a new method of using high-resolution microscopy to capture images of skin lesions on a low-cost mobile device. It can help improve diagnosis of a variety of skin conditions, including HIV-associated cancers, globally and in the U.S.
 Young Kim (in the foreground with his back to the camera) takes a photo using a smartphone of the inner eyelid of a study participant.
Young Kim (in the foreground with his back to the camera) takes a photo using a smartphone of the inner eyelid of a study participant.
2. Indiana researcher develops app to detect anemia in low-resource settings
Dr. Young Kim from Purdue University, West Lafayette, Indiana, and his colleagues at Moi Teaching and Referral Hospital and the AMPATH program in Kenya used their Fogarty’s Mobile Health (mHealth) award to develop an app that can detect anemia and sickle cell disease from a photo of a patient’s inner eyelid. Dr. Kim's startup is now adapting this technology to the U.S.
3. Mobile app for management of hypertension and diabetes in under-resourced communities
Dr. Annette L Fitzpatrick, Research Professor Emeritus at University of Washington, Seattle, is using her Fogarty mHealth award to develop a mobile health communications application for self-management of hypertension and diabetes and to test it in rural and urban-poverty communities in Cambodia. The conditions her study aims to address are important contributors to morbidity and mortality in the U.S. and the app could help improve their management in under-resourced rural and urban areas.
Harnessing unique research opportunities abroad to address common challenges in chronic, noncommunicable diseases
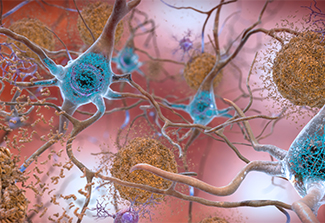 Beta-amyloid plaques and tau in the brain, abnormalities that are considered some of the main features of Alzheimer’s disease.
Beta-amyloid plaques and tau in the brain, abnormalities that are considered some of the main features of Alzheimer’s disease.
1. Alzheimer’s disease: University of Texas researcher explores condition in Hispanic population while Fogarty-trained scientists study a unique cohort in Columbia
Dr. Gladys Maestre, a Fogarty-funded researcher at The University of Texas Rio Grande Valley has conducted research in Venezuela and other countries, as well as in the U.S., to investigate cultural, educational, and genetic risks of Alzheimer’s disease (AD) and cognitive decline. She combines the strength of a Texas AD cohort, whose access to advanced care in U.S. allows for detailed clinical, neuroimaging, and genomic characterization, with a patient cohort in Venezuela, uniquely uniform in both inheritance and environmental exposures. Using this group, researchers can identify gene variants associated with specific manifestations of AD. Dr. Maestre also supports the training of early-career investigators, aiming to advance the study of Alzheimer’s disease and related disorders in Hispanics both in the U.S. and abroad.
Colombia is home to the largest known family with an inherited, early-onset form of Alzheimer’s disease. Its members participated in an innovative Alzheimer's prevention trial to determine if a drug developed by a U.S.-based company can stave off the decline in brain function associated with the disease. A recent genetic
study in the population has identified a mutation that delays the onset of the symptoms. Fogarty helped set the stage for these studies by supporting the training of local scientists in cutting-edge neuroscience methods.
2. Transforming care for a life-threatening pediatric condition
Dr. Benjamin Warf, a grantee of Fogarty’s
Global Brain and Nervous System Disorders Research across the Lifespan program and recipient of the 2012 McArthur genius award, partnered with the CURE pediatric neurosurgery hospital in Mbale, Uganda, to developed and test a novel treatment for hydrocephalus, a life-threatening build-up of excess fluid in the brain that occurs in about one or two out of every 1,000 babies born in the US. In partnership with his Uganda colleagues’, his research can help reduce the cost of caring for the condition--and could save patients’ lives--in both resource-poor and wealthy countries.
3. Affordable technology to prevent common diabetes complication
Dr. Jaime Miranda of Universidad Peruana Cayetano Heredia, Lima, Peru is using Fogarty support to develop an intervention that combines an inexpensive device to measure skin warmth at home with an SMS reminder to help patients with diabetes monitor for diabetic foot neuropathy, a common complication putting them at risk for foot amputation.
Investing in partnerships to protect against pandemic threats
-edit.jpg) A picture taken on October 1, 2013, shows people waiting to be screened as part of protective measures against the Ebola virus, next to a warning sign at a border crossing with Sierra Leone in Liberia's western Cape Mount province, the country's first province to be quarantined.
A picture taken on October 1, 2013, shows people waiting to be screened as part of protective measures against the Ebola virus, next to a warning sign at a border crossing with Sierra Leone in Liberia's western Cape Mount province, the country's first province to be quarantined.
Recent epidemics of Ebola and COVID-19 highlight the need for a critical mass of well-trained scientists and health research professionals capable of responding--efficiently and in a timely manner--to emerging infectious diseases outbreaks. The Mali-Guinea Emerging Infectious Disease Research Training Program, supported by Johns Hopkins University and NIH (FIC/NIAID), offers high-level training in field and laboratory epidemiology, translational clinical research, public health emergency management, and genomic characterization and surveillance of emerging infectious pathogens. The program grew out of a collaboration between the two nations during the early response to the Ebola epidemic: as the outbreak started in Guinea, Mali provided early support to its neighbor and, as result, was able to contain the virus faster within its own borders. The training will contribute to a more coordinated cross-border approach to public health preparedness and response that will help prevent the spread of emerging infections to the U.S.
Modeling disease to inform pandemic preparedness and response
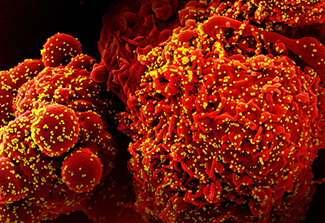 A scan of an electron micrograph of a cell infected with the Omicron strain of SARS-CoV-2 virus particles.
A scan of an electron micrograph of a cell infected with the Omicron strain of SARS-CoV-2 virus particles.
Fogarty's Division of International Epidemiology & Population Studies (DIEPS) supports pandemic preparedness and response in the U.S. through research and training on epidemiological modeling and genomic epidemiology. A recent study co-authored by Drs. Amanda Perofsky and Cecile Viboud of DIEPS analyzed viral genetic sequences to identify geographic differences in the transmission of SARS-CoV-2 in a large US metropolitan county. The analysis revealed increased local transmission and viral persistence in the Southern part of the county, linked to population mobility patterns. Authors’ results can inform decision-making at a local scale in the U.S.
Another DIEPS researcher, Dr. Nídia Trovão, has trained international scientists who lack access to a robust technological infrastructure to use a portable genomic sequencing platform to generate full SARS-CoV-2 genomes, create genomic databases, and study virus’ mutation patterns and evolutionary dynamics. This knowledge should help researchers better understand viral dynamics within their countries, enabling them to implement more efficient containment strategies without dependence on international assistance.
More information
Updated April 10, 2025