Studying COVID-19 in South Africa sheds light on how immunity contributes to variant success
November/December 2023 | Volume 22 Number 6
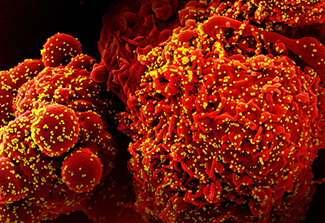 Image courtesy of NIAIDColorized scanning electron micrograph of a cell (red) infected with the Omicron strain of SARS-CoV-2 virus particles (yellow), isolated from a patient sample.
Image courtesy of NIAIDColorized scanning electron micrograph of a cell (red) infected with the Omicron strain of SARS-CoV-2 virus particles (yellow), isolated from a patient sample.
First author Dr. Kaiyuan Sun was joined by Dr. Cécile Viboud and colleagues from the CDC, Johns Hopkins University, and South African academies and institutions for this Nature Communications' study.
SARS-CoV-2's rapid evolution throughout the pandemic has been one of the virus' most prominent features. Every few months new variants have emerged to become dominant globally. To date, the World Health Organization has classified five SARS-CoV-2 lineages as variants of concern (VOCs), including Alpha, Beta, Gamma, Delta and Omicron. The selective advantage of each new variant (and its subvariants) is shaped in part by host population immunity. As of August 1, 2022, South Africa had experienced five SARS-CoV-2 epidemic waves. Scientists suggest the Beta VOC and Omicron subvariants BA.1, BA.4 and BA.5 are likely to have emerged in the region. For this reason, detailed studies of South Africa's immunologic landscape could provide a unique perspective on how immunity contributes to variant success.
For data, the authors turned to a prospective study of roughly 200 randomly selected South African households, half of which live in a rural community in Mpumalanga Province, the other half in an urban community in North West Province. Participants in the PHIRST-C study—the Prospective Household study of SARS-CoV-2, Influenza, and Respiratory Syncytial virus community burden, Transmission dynamics and viral interaction in South Africa study—were visited twice-weekly for collection of nasal swabs and information on symptoms, and every two months for blood draws. PHIRST-C seeks to answer various questions, including: Who is most at risk for severe illness? Can asymptomatic individuals transmit the virus? How is SARS-CoV-2 influenced by other respiratory viruses, including flu? How do age and HIV-infection affect transmission and symptoms?
Sun and his co-authors quantified changes in the immunologic exposure to SARS-CoV-2 across the population and over time and compared Omicron's epidemiology to that of prior variants. The team found the Omicron wave infected 58% and 65% of the population in the study's urban and rural cohorts, respectively. Reinfections and vaccine breakthrough infections accounted for more than half of the Omicron infections, the researchers noted. After adjusting for prior immunity and other factors, they estimated that people were more than twice as likely to get infected during Omicron than Delta; and relaxing nonpharmaceutical interventions likely contributed to this higher risk. Overall, the Omicron wave had a significantly higher attack rate in South Africa, compared to previously circulating strains. Dr. David Spiro, director of Fogarty's Division of International Epidemiology and Population Studies, commented: "This study showcases some of the cutting-edge research recognized as typical of our team by others in the field."
Updated December 5, 2023
To view Adobe PDF files,
download current, free accessible plug-ins from Adobe's website.
Related World Regions / Countries